Case Report - (2022) Volume 10, Issue 1
Subacute thyroiditis in a patient with HIV
Seow Chu Ee* and Lee Ze Chen2Department of Medicine, National University of Ireland, Selayang Hospital, Penang, Malaysia
Received: 03-Mar-2022, Manuscript No. MACR-22-55533; Editor assigned: 05-Mar-2022, Pre QC No. MACR-22-55533 (PQ); Reviewed: 20-Mar-2022, QC No. MACR-22-55533; Revised: 24-Mar-2022, Manuscript No. MACR-22-55533 (R); Published: 07-Apr-2022, DOI: 10.51268/ 2736-1888-22.10.132
Abstract
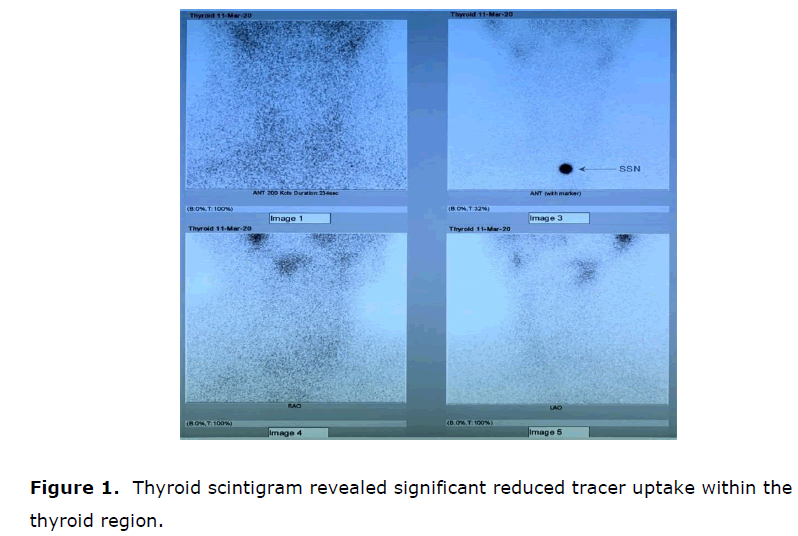
Transient hyperthyroidism can be part of the presentation for subacute thyroiditis, with a classic triphasic course (thyrotoxicosis, hypothyroidism, recovery). This is a case of a 46 year old male diagnosed with Human Immunodeficiency Virus (HIV) infection on Highly Active Antiretroviral Therapy (HAART), presented with prodrome of fever and malaise, followed by sore throat and tender, swollen thyroid. He had hyperthyroid symptoms on initial presentation as well. Thyroid function test showed hyperthyroidism. Inflammatory markers Erythrocyte Sedimentation Rate (ESR) and C Reactive Protein (CRP) were elevated. Ultrasound neck excluded presence of collection, thyroid scintigram revealed significant reduce tracer uptake within the thyroid region, consistent with diagnosis of subacute thyroiditis. He was treated with T Ibuprofen and oral Propranolol. Hyperthyroid symptoms, fever, thyroid pain and swelling were resolved in subsequent clinic review, with latest thyroid function test showing hypothyroidism. It is crucial to identify subacute thyroiditis with thyroxicosis as the initial presentation. This is because the management is different from other causes hyperthyroidism, where antithyroid drug is always unnecessary in managing the transient thyrotoxicosis.
Keywords
Transient hyperthyroidism, Subacute thyroiditis, Recovery, Pain, Treatment.
Introduction
Hyperthyroidism is the state of inappropriately high synthesis and secretion of thyroid hormones by the thyroid gland. Among coastal communities of Malaysia, Shahar MA et al. reported the prevalence of overt and subclinical hyperthyroidism was 3.4 and 26.8 per 1000 population respectively (Shahar MA et al., 2016). Grave’s disease, toxic multinodular goiter, and toxic adenoma are the common causes of hyperthyroidism. Transient hyperthyroidism can be part of the presentation for subacute thyroiditis, with a classic triphasic course of thyrotoxicosis, followed by hypothyroidism and recovery. Other type of thyroiditis includes painless (silent) thyroiditis, acute (suppurative) thyroiditis, palpation (traumatic) thyroiditis, postpartum thyroiditis, and drug-induced thyroiditis (Ross DS et al., 2016).
Thyroid disorder is not uncommon among individuals infected with HIV. The prevalence of abnormalities in thyroid function tests among HIV patients ranges from 12.6 to 19% (Madeddu G et al., 2006; Kaneria M et al., 2016) In view of the underlying immune compromised state, systemic opportunistic conditions that can infect or infiltrate the thyroid gland need to be considered as possible differential diagnosis for thyroiditis among HIV-infected individuals. Pneumocystis jiroveci infection, Cryptococcus neoformans infection, visceral leishmaniasis, suppurative bacterial infection of thyroid as well as other viral infection [Cytomegalovirus (CMV), Epstein Barr Virus (EBV), mumps and Enterovirus] have been reported in association with thyroiditis (Mayer KH et al., 2007; Desailloud R et al., 2009) It is important to identify subacute thyroiditis which can present with thyroxicosis in the initial phase, as the management is different from other etiologies hyperthyroidism.
Case Description
This is a case of a 46 year old male diagnosed with HIV infection in November 2015, had HAART initiated in June 2016 with Emtricitabine-Tenofovir disoproxil fumarate and Efavirenz. Compliance to HAART is good, with latest CD4 count of 349/mm3, and HIV viral load of less than 20 copies/ml. He had history of hepatitis C in December 2013, achieved Sustained Virologic Response (SVR) after completed 24 weeks of Peg interferon alfa-2a and Ribavirin.
He presented to emergency unit of Penang Hospital with two weeks history of low-grade fever and malaise, followed by one week history of swelling and pain over anterior neck associated with sore throat. He also experienced hyperthyroid symptoms, including sweating, heat intolerance, palpitation, and on and off loose stool. There was no history of cough, flu, shortness of breath, vomiting or abdominal pain. Drug history was unremarkable, except for antiviral agents patient been taking since June 2016. There is no history of radiation or trauma to the neck region. On examination, he is not tachynoeic, septic or agitated, temperature 38.3°C, heart rate 102 beats/min with regular pulse, other vital signs were stable. His thyroid was diffusely enlarged and firm, with tenderness on palpation. There was no thyroid eye sign and tremor.
Throat was injected; chest, cardiovascular and per abdomen examination were unremarkable. Complete blood count showed a white blood cell count of the 7.9 × 103/μL (80% neutrophils), hemoglobin of 10.9g/dl, and a platelet count of 422 × 103/μL. Other blood test results on initial encounter including thyroid stimulating hormone (TSH), 0.01mIU/ml (normal range 0.27 to 4.20 m IU/ml); Free Thyroxine (fT4), 41pmol/L (normal range, 12 to 22pmol/L); erythrocyte sedimentation rate, 75mm/hour (normal level, 0 to 10mm/hour); and C Reactive Protein (CRP) 203.8mg/L (normal range,<5mg/L). Liver function tests and renal profile were normal. Electrocardiogram (ECG) showed sinus tachycardia, chest x ray was unremarkable with clear lung fields.
Ultrasound of neck was arranged after admission to ward, showing bilateral thyroid nodules without hypodense lesion to suggest presence of collection. There was no increased vascularity on color Doppler and no significant cervical lymphadenopathy.
Scintigram of thyroid on the other hand revealed significant reduce tracer uptake within the thyroid region. Scan finding is likely due to acute thyroiditis in correlation with clinical presentation. TSH Receptor Autoantibodies (TRAb) and Thyroid Peroxidase (TPO) antibody were sent, both turned up to be negative.
Oral Amoxicillin Clavulanate (Augmentin) was started in ward in light of pharyngitis. T Ibuprofen was started as well. He was also placed on propranolol for the features of thyrotoxicosis. He was discharged home on day 6 of admission with oral Ibuprofen as needed for analgesic purpose. He is doing well during his subsequent review under Endocrine clinic with resolved hyperthyroid symptoms, fever, thyroid pain and swelling. TSH, T4, ESR, CRP trend were shown in Tables 1 and 2 and Figure 1.
| Weeks | TSH (mIU/ml) | fT4 (pmol/L) |
|---|---|---|
| 0 | 0.1 | 41 |
| 1 | 0.1 | 29 |
| 3 | 0.58 | 8 |
| 7 | 3.61 | 9 |
| Weeks | ESR (mm/hr) | CRP (mg/L) |
|---|---|---|
| 0 | 75 | 203.8 |
| 1 | 85 | 105.9 |
| 3 | 26 | 9.7 |
| 7 | 3 | 1.3 |
Results and Discussion
Subacute thyroiditis is one of the common causes of thyroid pain, most often occurs at 40 to 50 years of age (Ross DS et al., 2016). In this case, clinical suspicion of subacute thyroiditis was made base on prodrome of fever and malaise followed by thyroid pain. Subacute thyroiditis generally presents after a viral upper respiratory tract infection, commonly within the past 30 days (Ross DS et al., 2016; Fatourechi V et al., 2003). CMV, Coxsackie virus, influenza virus, adenovirus, EBV, and herpes simplex virus have been reported in association with subacute thyroiditis (Desailloud R et al., 2009). Symptoms of pharyngitis occurred at the same time with thyroid pain in this case. Patient also experience hyperthyroid symptoms such as sweating, heat intolerance, palpitation, and on and off loose stool. Thyroid function test showed hyperthyroid status with elevated fT4 and suppressed TSH. Approximately 50% of patients with subacute thyroiditis have an initial phase of hyperthyroidism (Ross DS et al., 2016; Bindra A et al., 2008). This happens as the result of damaged thyroid follicular cells by activated cytotoxic T lymphocytes, causing unregulated release of preformed thyroid hormones into the circulation. The diagnosis of subacute thyroiditis was supported by raised ESR and CRP, as well as other imaging studies discussed below. Negative history of radiation and trauma to the neck area, with no recent intake of new drugs especially Amiodarone, interferon-alfa, interleukin-2, and lithium making the differential diagnosis of radiation, trauma or drug induced thyroiditis less likely (Bindra A et al., 2008). Ultrasound of neck was performed to exclude presence of intrathyroidal collection or ill-defined hypoechoic areas of low vascularization which is commonly seen in cases of acute suppurative thyroiditis (Takahashi MS et al., 2019) Presentation of acute suppurative thyroiditis can mimic subacute thyroiditis with the presence of fever and swollen, tender thyroid, thus need to be excluded particularly in this case where patient is immune compromised. This is important as fine-needle aspiration of the lesion with parenteral antibiotics coverage is necessary in the case of acute suppurative thyroiditis, and surgical drainage may be required as well. In this case, intra thyroidal collection was not detected during ultrasound of the neck. There was no increase vascularity on color Doppler of thyroid gland, suggestive of subacute phase of thyroiditis, as acute phase of thyroiditis often shows diffuse hyper vascularization of thyroid gland (Bindra A et al., 2008). Thyroid scintigram on the other hand showed significant reduce tracer uptake within the thyroid region. Low radioiodine uptake in the context of hyperthyroid status is in favour of the diagnosis of subacute thyroiditis. In this case, postviral subacute thyroiditis is likely with the presence of pharyngitis (Ross DS et al., 2016; Mayer KH et al., 2007; Bindra A et al., 2008).
Beta blockers and anti-inflammatory therapy remains the mainstay of treatment for subacute thyroiditis (Ross DS et al., 2016). T Propranolol 20mg BD was started to control thyrotoxic symptoms. T Ibuprofen was prescribed to alleviate pain in this case, which is also the first line therapy for subacute thyroiditis. Corticosteroid therapy should be initiated if patient fail to respond to full doses of No steroidal Anti-Inflammatory Drugs (NSAIDs) over several days. Fortunately, patient’s symptoms controlled with T Ibuprofen and he was discharged home uneventful on day 6 of admission. With NSAIDs, the median time for the resolution of pain is about 5 weeks. Unlike other etiologies of hyperthyroidism, antithyroid drugs have no role in the treatment of subacute thyroiditis (Ross DS et al., 2016). Hyperthyroidism state in subacute thyroiditis is usually transient, enduring for three to six weeks and ceasing when the thyroid stores are exhausted. During the follow up sessions in endocrine clinic, patient reported resolution of fever as well as significant reduction in thyroid pain and swelling. Clinically, he is euthyroid even though latest repeated thyroid function test shows reduced fT4, consistent with hypothyroidism which might happen in 34 to 60% of subacute thyroiditis patients within the first 12 months (Fatourechi V et al., 2003; Benbassat CA et al., 2007) Both ESR and CRP were normalized by week 7. Anyway, thyroid function tests need to be monitored continuously in successive clinic reviews, as permanent hypothyroidism develops in approximately 10% of patients with subacute thyroiditis, where by thyroxine replacement is required. Study by Takahashi MS et al. shows subacute thyroiditis patients with hypothyroid phase tend to have antithyroid antibodies at baseline (Benbassat CA et al., 2007). Both TRAb and TPO antibodies were absent in this case (Fatourechi V et al., 2003). reported 4% of recurrence rate amongst patient with subacute thyroiditis.
Conclusion
This case highlights the importance of diagnosing subacute thyroiditis in patient presenting with hyperthyroidism, and tender, swollen thyroid gland from careful history taking, clinical examination, as well as imaging studies. Both ultrasound of neck and thyroid scintigram play a significant role in excluding other causes of thyroiditis. Beta blockers and anti-inflammatory therapy remains the mainstay of treatment for subacute thyroiditis, where antithyroid drugs has limited role in managing the transient thyrotoxicosis. Thyroid function tests should be performed from time to time in subsequent clinic visits to monitor complication of permanent hypothyroidism, where thyroxine replacement might be required.
REFERENCES
Shahar MA, Saud Gany SL, Omar AM, Abdul Wahab N, Sukor N, Kamaruddin NA. Prevalence of thyroid dysfunction in east and west coast of malaysia. J Endocrinol Metab. 2016:41
Ross DS, Burch HB, Cooper DS, Greenlee MC, Laurberg P, Maia AL. American thyroid association guidelines for diagnosis and management of hyperthyroidism and other causes of thyrotoxicosis. Thyroid. 2016; 26:1342-1343. [Crossref] [Google Scholar] [PubMed]
Madeddu G, Spanu A, Chessa F, Calia GM, Lovigu C, Solinas P. Thyroid function in human immunodeficiency virus patients treated with highly active antiretroviral therapy (Haart): a longitudinal study. Clin Endocrinol. 2006; 64(4): 375-383. [Crosseref] [PubMed] [Google Scholar]
Kaneria M, Kahalekar V. A study of thyroid dysfunction in HIV infected patients in a tertiary care hospital. Int J Adv Med. 2016; 3(3): 708-715. [Cross Ref] [Google Scholar] [PubMed]
Mayer KH, Hoffmann CJ, Brown TT. Thyroid function abnormalities in hiv-infected patients. Clin Infect Dis. 2007; 45(4):488-494. [Crossref] [Google Scholar] [PubMed]
Desailloud R, Hober D. Viruses and thyroiditis: an update. Virol J. 2009; 6(1):5. [Crossref] [Google Scholar] [PubMed]
Fatourechi V, Aniszewski JP, Fatourechi GZE, Atkinson EJ, Jacobsen SJ. Clinical features and outcome of subacute thyroiditis in an incidence cohort: olmsted county, minnesota, study. J Clin Endocrinol Metab. 2003; 88(5): 2100-2105. [Crossref] [Google Scholar] [PubMed]
Bindra A, Braunstein G.D. Thyroiditis. Am Fam Physician. 2006; 73(10): 1769-1776. [Crossref] [Google Scholar] [PubMed]
Takahashi MS, Pedro HM Moraes, Chammas MC. Ultrasound Evaluation of Thyroiditis: A Review. J Laryngol Otol. 2019; 2(1):127.
Benbassat CA, Olchovsky D, Tsvetov G, Shimon I. Subacute thyroiditis: Clinical characteristics and treatment outcome in fifty-six consecutive patients diagnosed between 1999 and 2005. J Endocrinol Invest 2007; 30(8): 631-635. [Crossref][Google Scholar] [PubMed]