Research Article - (2022) Volume 10, Issue 3
Adherence to healthy lifestyle behaviours and associated factors among hypertensive patients in bahir dar city, northwest Ethiopia
Mulualem Gete Feleke1*, Tesfaye Yitna1, Tamiru Alene2, Moges Wubneh3 and Nigusie Solomon32Department of Pediatrics Nursing, College of Health Sciences, University of Injibara, Injibara, Ethiopia
3Department of Health Sciences, College of Health Sciences and Medicine, University of Debre Tabor, Debre Tabor, Ethiopia
Received: 16-Jul-2022, Manuscript No. AERR-22-69370; Editor assigned: 18-Jul-2022, Pre QC No. AERR-22-69370 (PQ); Reviewed: 01-Aug-2022, QC No. AERR-22-69370; Revised: 18-Aug-2022, Manuscript No. AERR-22-69370 (R); Published: 28-Aug-2022, DOI: 10.51268/2736-1853.22.10.067
Abstract
Background: In recent decades, the issue of adherence to lifestyle modifications is one of the keys to improving blood pressure control. Although lifestyle modification is a strong recommendation for the prevention and treatment of hypertension, little is known about the hindering and provoking factors with adherence to the recommended lifestyle modification in Ethiopia, particularly in Bahir Dar City. Therefore, this study aimed to investigate factors associated with the recommended lifestyle behaviours among people with hypertension in Bahir Dar City.
Methods: A cross-sectional study was conducted at Bahir Dar city governmental hospitals from February-March 2020. Proportional allocation and systematic random sampling techniques were used. Data was collected through face-to-face interviews and clients’ chart reviews. The logistic regression model was used to assess the association between predictors and adherence to lifestyle modification. The association was interpreted using the odds ratio and 95% confidence interval.
Results: The result of 375 respondents included in this study, 210 (56%) were male. The mean age of the participants was 52.8 years. The proportion of adherence to healthy lifestyle modification was 14.9% (CI: 11.3, 18.4). Educational level college and above (AOR=7.6, CI=1.65, 34.81), knowledgeable about hypertension (AOR=4.8, CI=1.84, 12.27), measuring of blood pressure only on appointment date (AOR=0.2, CI=0.03, 0.64), and had strong social support (AOR=7.1, CI=2.85, 17.46) were adherence to lifestyle modification.
Conclusion: This study demonstrated that participants have low adherence to healthy lifestyle modification. Therefore, availed a social network of family and friends; providing healthy lifestyle education to address the participants’ knowledge of hypertension is an integral part of overall health in people with hypertension.
Keywords
Adherence, Healthy lifestyle, Hypertension.
Introduction
The ultimate goal of hypertension treatment is to control Blood Pressure (BP) to less than 130/80 millimetres of mercury (Whelton et al., 2018; Carey et al., 2018). Well-controlled BP has been associated with the mean reductions of more than 50% in the incidence of heart failure, more than 20% in the myocardial infarction, more than 14% (11%-17%) in chronic heart disease, and also more than 18% (15%-18%) in the stroke (Salam et al., 2019; Edgar et al., 2009). Lifestyle or behavioural factors critically determine the level of BP in individuals and the prevalence of hypertension in the population (Casey et al., 2019). A substantial body of evidence strongly supports the concept that lifestyle modification can have powerful effects on BP (Appel, 2003). Lifestyle modification has important roles in hypertensive people for first-line therapy, adjunct to drug therapy, and facilitating drug step-down or withdrawal (Appel, 2003).
Current recommendations for the prevention and treatment of high BP emphasize healthy lifestyle modification (Forman et al., 2009). Increase physical activity (exercising 3 or 4 times per week for an average of 40 minutes per session), reduced salt intake (less than 2,400 mg per day), increase potassium intake (2100 mg per day), and overall healthy dietary pattern, termed the Dietary Approaches to Stop Hypertension (DASH) diet, effectively lower BP. The DASH diet emphasizes fruits, vegetables, and low-fat dairy products and reduces fat and cholesterol (Casey et al., 2019).
Long-established lifestyle modifications that effectively lower BP include weight loss, reduced sodium intake, increased physical activity, smoking cessation, and limited alcohol consumption. Excess body fat is a predominant cause of hypertension with additive effects of dietary salt, alcohol, and physical inactivity (Oza et al., 2015; Robbins et al., 2011). The adoption of a healthy lifestyle by all individuals is critical in the prevention and an indispensable part of the management of those people with hypertension. Adhere to the DASH diet is decreased the Systolic and Diastolic Blood Pressure by 11 mm Hg and 3 mm Hg respectively. Low salt consumption also decreased SBP by 5-6 mmHg and DBP by 2-3 mmHg (Bakris et al., 2019).
There are many gaps in our current knowledge about the adoption of lifestyle change behaviours in hypertension people. Adherence to healthy lifestyle behaviours varied from country to country. Previous studies showed that adherence to lifestyle modifications was 1.7 % in Columbia, 44.1 in Kenya, 27.79% in Iran, 23% in Jordan, and 72% in Ghana (Fang et al., 2016; Kimani et al., 2019; Akbarpour et al., 2018; Alefan et al., 2019; Obirikorang et al., 2018). It is also varied widely from place to place in Ethiopia. For instance, the overall adherence to recommended healthy life were 23% in Addis Ababa, 62.1% in Harar, 27.3% in south Ethiopia, 59.4% in Gondar, 33.3% - 68.92% in Oromia, and 20.3% in Tigray region (Tibebu et al., 2017; Nadewu et al., 2018; Buda et al., 2017; Worku et al., 2020; Angelo et al., 2020; Fetensa et al., 2019; Gebremichael et al., 2019).
Socio-demographic factors that had a significant association with adherence to lifestyle behaviour among people with hypertension were; sex, age, educational level, marital status, occupational status, income, and residency were significantly associated with adherence to healthy lifestyle modification (Alefan et al., 2019; Tibebu et al., 2017; Gebremichael et al., 2019; Buda et al., 2017; Angelo et al., 2020; Fetensa et al., 2019; Obirikorang et al., 2018; Nadewu et al., 2018; Hareri et al., 2013; Asgedom et al., 2020).
Clinical factors which were statistically associated with adherence to recommended healthy lifestyle modification among people with hypertension were; duration of hypertension, knowledge of hypertension, and information about healthy lifestyle, adherence to treatment, health care facility access, present of comorbidity, frequency of hospital visit, lack of self-management counselling (Alefan et al., 2019; Tibebu et al., 2017; Buda et al., 2017; Angelo et al., 2020; Gebremichael et al., 2019; Hareri et al., 2013; Nadewu et al., 2018; Asgedom et al., 2020). Behavioural related factors such as social inhibition were negatively affected in life, self-efficacy, and khat chewing habit influenced adherence to the recommended healthy lifestyle modification in people with hypertension (Alefan et al., 2019; Angelo et al., 2020; Asgedom et al., 2020; Tibebu et al., 2017; Nadewu et al., 2018).
Findings from this study will assist hospital staff in better management of hypertension and create patient awareness of dietary adherence. This will reduce the patient's load in the clinic, as well as morbidity and mortality that are associated with poorly controlled hypertension. The identification of gaps in the area of adherence to a healthy lifestyle among hypertensive patients can use a part of one input for policymakers to emphasize this neglected issue and the development of programs that play a key role in the complication of hypertension to maintain vital organ functions.
There have not been many published works on adherence to healthy lifestyle modification in Ethiopia. Though various studies on hypertension have been conducted with the knowledge and medication adherence, few studies have been carried out on adherence to healthy lifestyle modification in this region city administration.
Therefore, these findings cannot be generalized to the study area. Thus, this study aimed to assess the magnitude of adherence to healthy lifestyle behaviour and identify associated factors among people with hypertension in Bahir Dar city administration, Ethiopia.
Materials and Methods
Study area, period and design
This was a cross-sectional study conducted at Bahir Dar city from February 23th to March 23th 2020. The city has three governmental hospitals. These hospitals are Felege Hiwot Comprehensive Specialized Hospital (FHCSH), Addis-Alem General Hospital, and Tibebe Gihon Specialized Teaching Hospital (TGSTH). These hospitals are provided in-patient and out-patient services with the vision to provide quality and universal care delivery in the city to facilitate personal and regional development. In the outpatient, chronic followup department, approximately 790 adult people with hypertension (450 in FHCSH, 240 in Addis Alem, and 100 in TGSH) are seen monthly.
Study and source of population
All hypertensive patients on regular follow up in the government hospitals at Bahir Dar city administration were the source population, while all the selected hypertensive patients who fulfilled the inclusion criteria and were available during the time of data collection were the study population.
Inclusion and exclusion criteria
All people with hypertension aged ≥ 18 years, and who had been on regular follow up were included in this study, while those individuals who had the hearing and/or verbal impairment, and severe illness during the time of data collection were excluded from the study.
Sample size
The sample size was determined by using a single population proportion formula by considering the following assumptions: 95% (1.96) Confidence Interval (CI), 59.40% for adherence to healthy lifestyle modification, and 5% (0.05) marginal of error (Worku et al., 2020).
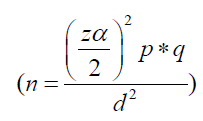
This yields an initial sample size of 351. By considering adjustment for the expected nonresponse rate (10%), the final sample size was 386 people with hypertension.
Study variables
Dependent variable: Adherence to healthy lifestyle behavior.
Independent variables: Socio-demographic factors (Age, sex, marital status, religion, and ethnicity, level of education, income, residence, occupation, and living arrangement).
Clinical factors (Comorbidities, knowledge about the hypertension, duration of hypertension, BMI, number of follow-up visits and number of antihypertensive medication, blood pressure measurement, family history, pay medication cost).
Social factors (Support from families and nonfamily members of the society).
Behavioral factors (alcohol consumption, smoking habit, exercise).
Sampling technique and procedure
Out of three public hospitals, that give hypertension follow-up services; all the three hospitals were selected conveniently. The numbers of study units from each hospital were proportionally allocated. Accordingly, 49, 213, and 113 cases were allocated proportionally to TGSTH, FCSH, and Adisalem hospital respectively, and then individual cases were recruited by a systematic random sampling procedure. After the first respondent was drawn by the lottery method, then every two intervals were interviewed until the sample size was reached.
Data collection tool and measurement
A well-reviewed and structured questionnaire was used to collect data. The questionnaires consisted of demographic information about hypertension knowledge, Body Mass Index (BMI), social support, and adherence to the recommended healthy lifestyle modification. To assess clinical related data: co-morbidity, duration of HTN since diagnosis, and previous blood pressure were collected from the clients’ charts by using checklists.
Adherence to the recommended healthy lifestyle modification was measured using questionnaires adapted from hypertension self-care management questions. This was recommended by the joint national committee on detection, prevention, evaluation, and treatment of hypertension and WHO STEPS questionnaires (Casey et al., 2019; Osako et al., 2017; Ukpabi et al., 2017). Adherence to lifestyle modifications by using the following dimension: (a) adherence to the dietary recommendation which consists of six components of diet items, such as salt restriction, low-fat diet, consumption of vegetables, fruits, whole grain, low-fat dairy products; and (b) adherence regarding the control of tobacco and alcohol (4 items), which was called “smoking and alcohol management,” and adherence to recommended physical activities.
Each item uses a 5-point Likert response scale except for physical activity: (1) never/very rarely, (2) rarely, (3) sometimes, (4) mostly, and (5) all of the time, with 1 to 5 points assigned, respectively, and reverse scores (saturated fat and sodium salt intake) are assigned for reverse questions (5–1 points). The dietary fruits, vegetables, whole grain, and low-fat dairy consumption were evaluated by asking how many times in the previous 7 days did the respondents eat the above-listed items. Those who responded “all” and “most times” were adherent while those who responded “sometimes”, “rarely”, or “none” were non-adherent. Dietary saturated fat and oil consumption was inquired about how many times in the previous 7 days the respondents ate. Those participants who responded “sometimes”, “rarely”, and “none” were considered adherent while those who responded “all”, and “most time” were nonadherent.
Salt consumption was also evaluated in the previous 7 days by inquiring about the addition of raw table salt in addition to the one used to prepare the food item during meal times. Those who responded “rarely” and “none” were considered adherent to recommended salt, whereas “all times”, “most times”, and “sometimes” were considered non-adherent to recommended dietary salt. Adherence to recommended physical exercise was also considered when the participants were exercised for ≥30 min per day; at least three times per week (Lee et al., 2011). Therefore, the overall adherence to the recommended healthy lifestyle modification was scored who fulfilled the entire components.
Knowledge about hypertension was assessed by Hypertension Knowledge-Level Scale (HKLS) questionnaires (Erkoc et al., 2012). This scale has 22 items that were used to assess respondents’ knowledge. It e contains parts of the definition, treatment, drug adherence, diet, lifestyle, and complications. The definition, lifestyle, diet, and complication part of the questionnaire was used to assess the knowledge of people with hypertension. The tool contains selected-response items with yes and no responses; the right answer is coded as “1” and the wrong answer is coded as “0”. Participants who scored equal to and above the mean value (7.2) on the hypertensive knowledge assessment scale were considered good knowledge. Participants who scored below the mean value (7.2) on the hypertensive knowledge assessment scale were considered poor knowledge.
People with hypertension who have supported by their families or friends or neighbors scored was assessed by the “Oslo 3-items social support scale.” The score ranged from 3-14. Participants who scored OSSS-3, (1) from 3-8 were considered poor socials support, (2) from 9-11 were considered moderate support, and (3) from 12-14 were considered strong support (Kocalevent et al., 2018).
Data quality control
Three BSc degree holder nurses for the data collection (one for each hospital) and three BSc degree holder’s supervision (one for each hospital) were recruited during the data collection period (both the data collectors and the supervisors were not from the same hospitals). At each hospital, the aim of the study was clearly explained to the study participants before they were interviewed. The data collectors and supervisors were trained in one day on how to facilitate the data collection process and prevent errors. The questionnaire checked for completeness, accuracy, and consistency by supervisors.
All the questions were prepared in English and translated into the Amharic language by an expert who was fluent in both languages and back-translated to English to see its consistency. Two weeks before the actual data collection, the questionnaires were pre-tested on 5% of the total sample among people with hypertension who had follow-ups at Debre Tabor hospital to evaluate the consistency and applicability of the questionnaire. The reliability of the questionnaire was evaluated using Cronbach's alpha test (α=0.76).
Data collection was preserved in a secure environment to avoid loss and breach of confidentiality. The supervisor and principal investigator closely followed the data collection process. Appropriate times to complete the questionnaire were allocated for the participants, and the completed questionnaires were collected timely.
Data processing and analysis
The collected data were entered, coded, and edited into EPI-data version 3.1, and exported to SPSS version 23 for analysis. Descriptive statistics were used to illustrate the means, standard deviations, medians, and frequencies of the study variables. Bivariate analysis was computed, and those variables whose p - values less than or equal to 0.2 were fitted into the backward stepwise multivariate logistic regression model. Odds ratios with 95% confidence interval were used to determine the strength of the association between dependent and independent variables.
The Hosmer and Lemeshow goodness of fit tests for the model were checked. Finally, the degree of association was interpreted by using the odds ratio with a 95% confidence interval. The P value of ≤ 0.05 was considered statistically significant.
Results
Socio-demographic characteristics of the participants
The 386 people with hypertension invited 375 participants in the study with a response rate of 97%. Of these, 210 (56%) were males. The mean age of the participants was 52.80 with a SD ± 11.52. Most of the participants, 310 (82.7%) were Orthodox Tewahido religion followers and 318 (84.8%) participants were from urban areas (Table 1).
| Variables | Categories | Frequency | Percent |
|---|---|---|---|
| Sex | Male | 210 | 56 |
| Female | 165 | 44 | |
| Age | 18-39 | 44 | 11.7 |
| 40-59 | 209 | 55.7 | |
| ≥ 60 | 122 | 32.5 | |
| Religion | Orthodox Tewahido | 310 | 82.7 |
| Muslim | 45 | 12 | |
| Protestant | 20 | 5.3 | |
| Ethnicity | Amhara | 359 | 95.7 |
| Tigre | 12 | 3.2 | |
| Other* | 4 | 1.1 | |
| Marital status | Single | 16 | 4..3 |
| Married | 286 | 6.3 | |
| Divorced | 42 | 11.2 | |
| Widowed | 31 | 8.3 | |
| Educational level | Unable to read and write | 93 | 24.8 |
| Able to read and write only | 52 | 13.9 | |
| Primary | 54 | 14.4 | |
| Secondary | 58 | 15.5 | |
| College and above | 118 | 31.5 | |
| Occupational status | Farmer | 51 | 13.6 |
| Housewife | 73 | 19.5 | |
| Governmental employee | 100 | 26.7 | |
| Private employee | 37 | 9.9 | |
| Merchant | 75 | 20 | |
| Retired | 33 | 8.8 | |
| Other** | 6 | 1.6 | |
| Average monthly income | ≤ 999 | 24 | 6.4 |
| 1000-1999 | 52 | 13.9 | |
| 2000-2999 | 68 | 18.1 | |
| ≥ 3000 | 231 | 61.6 | |
| Residence | Rural | 57 | 15.2 |
| Urban | 318 | 84.8 |
Note: *: level of significance.
Clinical characteristics of the study participants
About 153 (40.8%) participants lived with hypertension for ≥ four years and 277 (73.9%) of them had no family history of hypertension. Of the total enrolled participants, 196 (52.3%) of them had received education on hypertension and 166 (44.3%) had got overweight. Almost one-fourth (50.7%) of participants were knowledgeable about hypertension holding 7.25 for the mean score of knowledge. Nearly half (45.3%) of participants had comorbid diseases, of which, 49 (28.8%) of respondents had more than one comorbidities. The mean SBP and DBP of the study participants were 131.7 ± 16.95 and 80.5 ± 10.38 respectively. Of the total participants, 121 (32.3%) reported that they had strong social support (Table 2).
| Variables | Categories | Frequency | Percent |
|---|---|---|---|
| Family history of HTN | No | 277 | 73.9 |
| Yes | 98 | 26.1 | |
| Duration of HTN | in year Less than 2 years | 93 | 24.8 |
| 2-4 years | 129 | 34.4 | |
| >4 years | 153 | 40.8 | |
| Received nutritional education | No | 179 | 47.7 |
| Yes | 196 | 52.3 | |
| Knowledge of hypertension | Poor-knowledge | 185 | 49.3 |
| Good-knowledge | 190 | 50.7 | |
| Comorbidity | Yes | 170 | 45.3 |
| No | 205 | 54.7 | |
| Type of comorbidities | DM | 43 | 25.3 |
| Stroke | 24 | 14.1 | |
| Renal disease | 15 | 8.8 | |
| Cardiac disease | 27 | 15.9 | |
| More than one | 49 | 28.8 | |
| Others* | 12 | 7.1 | |
| Frequency of BP measurement | Daily | 20 | 5.3 |
| Weekly | 61 | 16.3 | |
| Monthly | 137 | 36.5 | |
| During a symptom of HTN | 75 | 20 | |
| Only appointment date | 82 | 21.9 | |
| Blood pressure status | Controlled | 200 | 53.3 |
| Uncontrolled | 175 | 46.7 | |
| Body mass index | Underweight | 2 | 0.5 |
| Normal weight | 167 | 44.5 | |
| Overweight | 166 | 44.3 | |
| Obese | 40 | 10.7 | |
| Social support | Strong | 121 | 32.3 |
| Moderate | 154 | 41.1 | |
| Poor | 100 | 26.6 |
Note: *: level of significance.
Adherence to healthy lifestyle behavior
In this study, the magnitude of adherence to healthy lifestyle modification was 14.9% (CI: 11.3, 18.4). In the case of each domain, these studies revealed that the majority of the participants were nonsmokers (98.7%) and adhere to alcohol consumption (91.2%). Less than half of the participants adhered to physical activity (41.9%) and diet (32.8%) (Table 3).
| Variable | Frequency | Percent | |
|---|---|---|---|
| Adherence to the recommended life style modifications | Adherent | 56 | 56 14.9 |
| Non-adherent | 319 | 85.1 | |
| Adherence to dietary recommendation | Adherent | 123 | 32.8 |
| Non-adherent | 252 | 67.2 | |
| Adherence to exercise recommendation | Adherent | 157 | 41.9 |
| Non-adherent | 218 | 58.1 | |
| Adherence to smoking cessations | Not smoked | 370 | 98.7 |
| Not ceased | 5 | 1.3 | |
| Adherence to the recommended alcohol consumption | Adhere | 342 | 91.2 |
| Non-adherence | 33 | 8.8 | |
| Salt intake reduction | Adherence | 299 | 79.9 |
| Non-adherence | 76 | 20.3 | |
| Maintenance of a normal weight | Adherence | 167 | 44.5 |
| Non-adherence | 208 | 55.5 | |
Factors associated with adherence to healthy lifestyle behavior
After adjusting potential confounders of other covariates, educational level, frequency of measuring blood pressure, knowledge about hypertension, and social support were found to be significantly associated with adherence to healthy lifestyle behaviour. Respondents who had college and above educational level were 7.6 times more likely to adhere to the overall healthy lifestyle modification than those who were unable to read and write (AOR=7.6, CI: (1.96, 34.81), P=0.009).
Those respondents who measured their blood pressure when they feel signs and symptoms only were 80% less likely to adhere to healthy lifestyle behaviour than those who were measured their blood pressure daily (AOR=0.2, CI: (0.06, 0.81), P=0.024). Those respondents who had good knowledge were 4.8 times more likely to be adherent to healthy lifestyle modification as compared to those who had poor knowledge (AOR=4.8, CI: (1.84, 12.27), P=0.001). Those respondents who had strong social support were 5.2 times more likely to be adherent to healthy lifestyle modification as compared to poor social support (AOR=5.2, CI: (1.44, 18.59), P<0.012) (Table 4).
| Variable | Adherence to lifestyle | Bivariate | Multivariable | ||
|---|---|---|---|---|---|
| Yes | No | COR (CI) | AOR (CI) | P-value | |
| Age | |||||
| 18-39 | 6 | 38 | 1 | 1 | |
| 40-59 | 42 | 167 | 1.6 (0 .63, 4.02) | 2.5 (0.89, 7.12) | 0.084 |
| ≥ 60 | 8 | 114 | 0.4 (0.15, 1.36) | 1.8 (0.49, 6.62) | 0.381 |
| Marital status | |||||
| Single | 3 | 13 | 1 | 1 | |
| Married | 48 | 238 | 0.87 (0.24, 3.19) | 0.7 (0.13, 3.33) | 0.608 |
| Divorced | 2 | 40 | 0.2 (0.03, 1.44 | 0.2 (0.02, 2.06) | 0.186 |
| Widowed | 3 | 28 | 0.5 (0.08, 2.62) | 1.9 (0.21, 17.09) | 0.575 |
| Educational level | |||||
| Can’t read and write | 2 | 91 | 1 | 1 | 0.078 |
| Can read and write | 3 | 49 | 2.8 (0.45, 17.24) | 3.0 (0.45, 20.59) | 0.253 |
| Grade 1-8 | 6 | 48 | 5. 7 (1.11, 29.26) | 4.4 (0.79, 24.26) | 0.092 |
| Grade 9-12 | 10 | 48 | 9.5 (2.0, 45.02) | 4.7 (0.91, 23.93) | 0.065 |
| Collage & above | 35 | 83 | 19.2 (4.48, 82.26 | 7.6 (1.65, 34.81) | 0.009 |
| Residence | |||||
| Rural | 2 | 55 | 1 | 1 | |
| Urban | 54 | 264 | 5.6 (1.33, 23.76) | 1.14 (0.18, 7.28) | 0.887 |
| Duration of hypertension | |||||
| <2 year | 10 | 83 | 1 | 1 | |
| 2 to 4 year | 30 | 99 | 2.5 (1.16, 5.45) | 1.1 (0.41, 2.617) | 0.952 |
| >4 year | 16 | 137 | 0.9 (0.42, 2.24) | 1.1 (0.41, 3.06) | 0.834 |
| Received education | |||||
| No | 12 | 167 | 1 | 1 | |
| Yes | 44 | 152 | 4.0 (2.05, 7.91) | 1.3 (0.55, 3.216 | 0.532 |
| Frequency Blood pressure measurement | |||||
| Daily | 9 | 11 | 1 | 1 | |
| Weekly | 15 | 46 | 0.4 (0.14, 1.15) | 0.3 (0.09, 1.00) | 0.05 |
| Monthly | 21 | 116 | 0.2 (0.08, 0.60) | 0.3 (0.09, 0.92) | 0.046 |
| Feeling Sign of disease | 7 | 68 | 0.1 (0.04, 0.41) | 0.2 (0.06, 0.81) | 0.024 |
| Appointment date | 4 | 78 | 0.1 (0.02, 0.24) | 0.2 (0.03, 0.64) | 0.011 |
| Knowledge | |||||
| Poor-knowledge | 6 | 179 | 1 | 1 | |
| Good-knowledge | 50 | 140 | 10.6 (4.44, 25.57) | 4.8 (1.84, 12.27) | <0.001 |
| Social support | |||||
| Poor | 3 | 97 | 1 | 1 | 0.014 |
| Moderate | 18 | 136 | 4.3 (1.23, 14.93) | 2.5 (0.66, 9.12) | 0.182 |
| Strong | 35 | 86 | 13.2 (3.91, 44.32) | 5.2 (1.44, 18.59) | 0.012 |
| Blood pressure status | |||||
| Controlled | 40 | 160 | 1 | 1 | |
| Uncontrolled | 16 | 159 | 0.4 (0.22, 0.75) | 1.9 (0.67, 5.289) | 0.233 |
| Comorbidities | |||||
| Yes | 12 | 158 | 1 | 1 | |
| No | 44 | 161 | 3.6 (1.83, 7.07) | 1.5 (0.68, 3.27) | 0.325 |
Discussion
The ultimate goal of the hypertension treatment is to control blood pressure to less than 130/80 mmHg (Whelton et al., 2018). Adoption of a healthy lifestyle is important in the management of hypertension. Lifestyle or behavioural factors critically determine the level of BP control in an individual and the prevalence of hypertension in a population (Casey et al., 2019). A substantial body of evidence strongly supports the concept that lifestyle modification can have powerful effects on BP controlled (Svetkey e al., 2005). This study aimed to assess the magnitude of adherence to healthy lifestyle modification and determinates among people with hypertension.
In this study, the overall adherence to healthy lifestyle behaviours was 14.9%. A similar finding was reported in Nigeria (14.1%), much higher than a study reported in Saudi Arabia (4.2%) and Columbia (1.7%), and much lower than the study reported in Ghana (72.0%), Iran (27.79%), Jordan (23%), and Addis Ababa (23%), Harar (62.1%) (Elbur, 2015; Fang et al., 2016; Obirikorang et al., 2018; Alefan et al., 2019; Tibebu et al., 2017; Nadewu et al., 2018). This discrepancy could be explained by methodological factors where the latter included a small sample of only male participants in Saudi Arabia. In Colombia, the health professional promoted the practice of curing medicine rather than a better preventive behaviour like a healthy lifestyle. That is why a scholar concluded that unhealthy habits in the health professional and attitudes that do not favor the promotion of healthy habits in their client and their community (Sanabria-Ferrand et al., 2007).
In the case of Ghana, The Ministry of Health Ghana launched adopted the concept of "Regenerative Health and Nutrition". Regenerative health and nutrition aimed to promote healthy lifestyles, dietary practices, and mother and child care practices that would help eliminate the many diseases that impact the health and well-being of Ghanaians. The improvement in healthy lifestyle behaviours among adult Ghanaians will help promote healthy living and potentially lead to a reduction in the prevalence of obesity among Ghanaians (especially in women) (Tagoe et al., 2011). In Addis Ababa, there may a day-to-day physical activity, moderate alcohol consumption, no smoking, and sufficient vegetable and fruit consumption; these four habits in combination can make a new lifestyle and healthy living habits.
In this study only 32.8% adhered to a healthy diet. This finding is higher than a study reported in Columbia (14.1%) and Korea (<20%) (Fang et al., 2016; Xiao et al., 2011). But, much lower than the previous studies reported in Hara (81.8%), Addis Ababa (64.7%), and Tigray (67.20%) (Nadewu et al., 2018; Hareri et al., 2013; Gebremichael et al., 2019).
There might be also due to the economic class, as the nation is more industrialized the chance of adhering to a diet decrease due to easy access of non-recommended diets in restaurant and hotels. The national difference, there might be due to basic knowledge, practice, and attitude about hypertension. In a study conducted in Bahir Dar, the level of knowledge and practice among people with hypertension was poor (35), meanwhile in Addis Ababa and Tigray practice were relatively good (Ayele et al., 2017; Bacha et al., 2019; Bayray et al., 2018).
Physical activity plays an important role in preventing and managing hypertension. It is a cost-effective, practical, and natural, not need sophisticated technology, and effective way of controlling hypertension (Ghadieh et al., 2015). Despite the recommendation that confirms the health benefits of physical activities in reducing and preventing diseases, evidence showed that an ample of people remain physically inactive (Perkovic et al., 2007; Rossi et al., 2012). The result of our study showed that 41.9% of participants had adhered to physical exercise. Similar study reported in Korea (47.3%), Israel (50%) and Columbia (46.6%) (Fang et al., 2016; Ayele et al., 2017; Heymann et al., 2011). The magnitude of this finding is higher than a study conducted in Addis Ababa (31.4%) and lower than in Hara (62.3%) (Tibebu et al., 2017; Nadewu et al., 2018). More educational programs and intervention measures for adhering to physical activity should be targeted at people with hypertension.
In this study, 91.2% of participants were adhered to alcohol consumption; 98.7% of participants were non-smokers, and 79.9% of the participants had adhered to salt intake (limit less than 5 g per day of dairy consumption). Our findings indicated that more than 90% of the participants were adherent to healthy lifestyle modifications related to smoking and alcohol abstinence. This finding is consistent with the study conducted in Tigray, non-smoker were 89.9%- 99.1% and alcohol abstainers were 67.2%- 68.8%, Harar non-smoker were 95.8%, and alcohol adherence was 98.5% (Gebremichael et al., 2019; Niriayo et al., 2019; Nadewu et al., 2018).
In contrast, a low proportion of adherence to low salt intake was 29% in Tigray, Ayder comprehensive specialized hospital, and less than 20% in Korea (Ayele et al., 2017; Niriayo et al., 2019). This variation could be due to the differences in sociocultural factors. Salt intake in Korea principally comes from homeprocessed foods or condiments added during cooking, which differs from the situation in our country. Sodium intake in Korea is high, with about half the population consuming >4000 mg/day, twice the recommended upper limit (Lee et al., 2013). Adherence to the recommended salt intake of fewer than 5 grams per day for adults helps to reduce blood pressure and risk of cardiovascular disease, stroke, and coronary heart attack. The principal benefit of lowering salt intake is a corresponding reduction in high blood pressure (World Health Organization, 2007).
In this study, 44.5% of the respondents maintain normal body weight which is supported by a study in Korea 50% and higher than the study in Tigray 21.45% (Ayele et al., 2017; Niriayo et al., 2019). However, this finding is lower than the study of Harar 56.4% (Nadewu et al., 2018). Maintaining a 3% to 5% weight loss can significantly reduce the risk of cardiovascular disease (Expert Panel et al., 2014; Harsha et al., 2008).
In this study, an increased level of literacy who are college and above are more likely to adhered to a healthy lifestyle as compared to less level of literacy who cannot read and write, read and write, and primary educated. A previous study done in Harar, Tigray, and Ghana suggested that participants with a higher level of literacy linked to better adhere to healthy lifestyle modification (Nadewu et al., 2018; Gebremichael et al., 2019; Obirikorang et al., 2018). This is because literacy is help to participate meaningfully and assertively in decisions that affect one’s healthy lifestyle. Literacy enables people to read their own world and to write their own healthy history and practice the recommended healthy lifestyle (Morrisroe, 2014).
Frequency of blood pressure is negatively affected the healthy lifestyle modification. In this study, participants who measured blood pressure when they feel sign and symptoms was less likely adhered to healthy lifestyle modification than those who are measured their blood pressure daily. It may be due to the positive association of daily blood pressure measurement is important to identify white coat hypertension, detect masked elevated blood pressure, provide valuable information regarding treatment outcomes, and effectively adjust healthy life modification as recommended.
Knowledge about hypertension was significantly associated with healthy lifestyle modification. Participants who had good knowledge were 4.8 times more likely to adhere to healthy lifestyle behaviour. This is supported by the study finding in Addis Ababa, Mizan Tepi, Tigray, and Jordan (Tibebu et al., 2017; Angelo et al., 2020; Fetensa et al., 2019; Alefan et al., 2019). The findings suggest that good knowledge of hypertension is linked to adherence to healthy lifestyle modification and an improvement in blood pressure control (Deji-Dada et al., 2019).
In this study, social support was significantly associated with adherence to healthy lifestyle modification. Participants who had strong social support from their families, neighbours, and friends were 5.2 times more likely to adhere to healthy lifestyle modification. This finding was consistent with studies conducted in Addis Ababa (Tibebu et al., 2017). This might be due to the effect of social support on emotional wellbeing (as in receiving love and empathy) and practical help (like the gift of money, assistance with recommended care).
Conclusion
In the current study, adherence to healthy life behaviour is 14.9%. This shows that adherence to healthy lifestyle behaviour is very low. Educational level, daily blood pressure measurement, knowledge about hypertension, and social support were found significantly associated with adherence to the recommended healthy lifestyle modification. To be promoted to optimal blood pressure control client-cantered care is essential. Therefore, the health care providers should be availed of a social network of family and friends and providing education about hypertension to produce positive impact for healthy lifestyle behaviour.
Funding
No external funding was obtained for this study. The administrators of Bahir Dar University indirectly supported this project and had no role in study design, data collection, data analysis, data interpretation, or writing the report. The corresponding author had full access to all data in the study and had responsibility for the decision to send for publication.
Informed Consent and Patient Details
This study was conducted after approval of the proposal by Bahir Dar University College of medicine and health sciences institutional review board committee. Before the actual data collection, ethical approval and clearance were obtained from this board. Permission and the supportive letter were obtained from the Amhara public health institute and each hospital medical director's office. Participation was voluntary information was also collected anonymously after obtaining written consent from each respondent by assuring confidentiality. The participants also told the objective of the study and the right to refuse, stops, or withdraw at any time of data collection. Finally, participants were informed that no incentive or harm for their participation in this study.
Availability of Data and Materials
All data are available in the manuscript.
Ethics Approval and Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Competing Interests
The authors declare that we have no competing interests.
Author Contributions
All authors made important contributions to the manuscript preparation. MG and TA conceived the study and involved in the design, conduct the research and drafted the manuscript. MW, NS, and TY analysis, interpret the data and review the manuscript. All authors read and approved the final version of the manuscript.
Acknowledgements
We would like to offer our in-depth gratitude to the data collectors, participants and hospital workers. We also acknowledge Bahir Dar and Wolaita Sodo Universities for indirectly supporting the collection of data.
References
Akbarpour S, Khalili D, Zeraati H, Mansournia MA, Ramezankhani A, Fotouhi A (2018). Healthy lifestyle behaviors and control of hypertension among adult hypertensive patients. Sci. Rep. 8(1):1-9. [Crossref] [Google Scholar] [Pub Med]
Alefan Q, Huwari D, Alshogran OY, Jarrah MI (2019). Factors affecting hypertensive patients’ compliance with healthy lifestyle. Patient Prefer Adherence. 13:577-585. [Crossref] [Google Scholar] [Pub Med]
Angelo AT, Geltore TE (2020). Lifestyle modification practice and associated factors among diagnosed hypertensive patients in Mizan Tepi University Teaching Hospital South west Ethiopia, 2019: Cross-sectional study. PAMJ-Clinical Medicine. 2(156). [Crossref] [Google Scholar]
Appel LJ (2003). Lifestyle modification as a means to prevent and treat high blood pressure. J. Am. Soc. Nephrol. 14(suppl 2):S99-102. [Crossref] [Google Scholar] [Pub Med]
Asgedom SW, Amanuel K, Gidey MT, Niriayo YL, Gidey K, Atey TM (2020). Treatment resistant hypertension among ambulatory hypertensive patients: A cross sectional study. Plos one. 15(4):e0232254. [Crossref] [Google Scholar]
Ayele SK, Abdurehman KS (2017). Prevalence and assessment of knowledge and practice towards hypertension among Bahir Dar City communities, 2016: A community based cross-sectional study. Int. J. Nurs. Midwifery. 9(3):33-40. [Crossref] [Google Scholar]
Bacha D, Abera H (2019). Knowledge, attitude and self-care practice towards control of hypertension among hypertensive patients on follow-up at St. Paul’s hospital, Addis Ababa. Ethiop. J. Health. Sci. 29(4):421-430. [Crossref] [Google Scholar] [Pub Med]
Bakris G, Ali W, Parati G (2019). ACC/AHA versus ESC/ESH on hypertension guidelines: JACC guideline comparison. J. Am. Coll. Cardiol. 73(23):3018-3026. [Crossref] [Google Scholar] [Pub Med]
Bayray A, Meles KG, Sibhatu Y (2018). Magnitude and risk factors for hypertension among public servants in Tigray, Ethiopia: A cross-sectional study. PLoS One. 13(10):e0204879. [Crossref] [Google Scholar] [Pub Med]
Buda ES, Hanfore LK, Fite RO, Buda AS (2017). Lifestyle modification practice and associated factors among diagnosed hypertensive patients in selected hospitals, South Ethiopia. Clin. Hypertens. 23(1):1-9. [Crossref] [Google Scholar] [Pub Med]
Carey RM, Whelton PK, 2017 ACC/AHA Hypertension Guideline Writing Committee* (2018). Prevention, detection, evaluation, and management of high blood pressure in adults: Synopsis of the 2017 American College of Cardiology/American Heart Association Hypertension Guideline. Ann. Intern. Med. 168(5):351-358. [Crossref] [Google Scholar] [Pub Med]
Casey Jr DE, Thomas RJ, Bhalla V, Commodore-Mensah Y, Heidenreich PA, Kolte D, Muntner P, Smith Jr SC, Spertus JA, Windle JR, Wozniak GD (2019). 2019 AHA/ACC clinical performance and quality measures for adults with high blood pressure: A report of the American College of Cardiology/American Heart Association Task Force on Performance Measures. Circ. Cardiovasc. Qual. Outcomes. 12(11):e000057. [Crossref] [Google Scholar] [Pub Med]
Deji-Dada OO, Aina FO, Solomon OA, Omosanya OE, Gabriel OE, Shabi MO (2019). The impact of knowledge of hypertension on blood pressure control among the elderly hypertensives attending a primary health care facility in Ekiti, South West Nigeria. Nigerian Journal of Family Practice. 10(2):39-47. [Google Scholar]
Elbur AI (2015). Level of adherence to lifestyle changes and medications among male hypertensive patients in two hospitals in Taif; Kingdom of Saudi Arabia. Int. J. Pharm. Pharm. Sci. 7(4):168-172. [Google Scholar]
Edgar VL, Jeffery SB, Allen RN (2009). Current diagnosis and treatment: Nephrology and hypertension. Chapter 55. Pregnancy and renal disease. [Google Scholar]
Erkoc SB, Isikli B, Metintas S, Kalyoncu C (2012). Hypertension Knowledge-Level Scale (HK-LS): A study on development, validity and reliability. Int. J. Environ. Res. Public. Health. 9(3):1018-1029. [Crossref] [Google Scholar] [Pub Med]
Expert Panel Members, Jensen MD, Ryan DH, Donato KA, Apovian CM, Ard JD, Comuzzie AG, Hu FB, Hubbard VS, Jakicic JM, Kushner RF (2014). Executive summary: Guidelines (2013) for the management of overweight and obesity in adults: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Obesity Society published by the Obesity Society and American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Based on a systematic review from the The Obesity Expert Panel, 2013. Obesity. 22(S2):S5-39. [Crossref] [Google Scholar] [Pub Med]
Fang J, Moore L, Loustalot F, Yang Q, Ayala C (2016). Reporting of adherence to healthy lifestyle behaviors among hypertensive adults in the 50 states and the District of Columbia, 2013. J. Am. Soc. Hypertens. 10(3):252-262.e3. [Crossref] [Google Scholar] [Pub Med]
Fetensa G, Milkiyas N, Besho M, Hasen T, Teshoma M, Wakuma B, Etefa W, Fayisa L (2019). Assessment of knowledge and practice of life style modification among hypertensive patients at Nekemte specialized hospital, western Oromia, Ethiopia: A cross-sectional study design. J. Cardiovasc. Dis. Diagn. 7(389):2. [Google Scholar]
Forman JP, Stampfer MJ, Curhan GC (2009). Diet and lifestyle risk factors associated with incident hypertension in women. Jama. 302(4):401-411. [Crossref] [Google Scholar] [Pub Med]
Gebremichael GB, Berhe KK, Beyene BG, Gebrekidan KB (2019). Self-care practices and associated factors among adult hypertensive patients in Ayder Comprehensive Specialized Hospital, Tigray, Ethiopia, 2018. BMC. Res. Notes. 12(1):1-6. [Crossref] [Google Scholar] [Pub Med]
Ghadieh AS, Saab B (2015). Evidence for exercise training in the management of hypertension in adults. Can. Fam. Physician. 61(3):233-239. [Google Scholar]
Hareri HA, Abebe M, Asefaw T (2013). Assessments of adherence to hypertension managements and its influencing factors among hypertensive patients attending black lion hospital chronic follow up unit, Addis Ababa, Ethiopia-a cross-sectional study. Int. J. Pharm. Sci. Res. 4(3):1086-1095. [Google Scholar]
Harsha DW, Bray GA (2008). Weight loss and blood pressure control (Pro). Hypertension. 51(6):1420-1425. [Crossref] [Google Scholar] [Pub Med]
Heymann AD, Gross R, Tabenkin H, Porter B, Porath A (2011). Factors associated with hypertensive patients' compliance with recommended lifestyle behaviors. Isr. Med. Assoc. J. 13(9):553-557. [Google Scholar] [Pub Med]
Kimani S, Mirie W, Chege M, Okube OT, Muniu S (2019). Association of lifestyle modification and pharmacological adherence on blood pressure control among patients with hypertension at Kenyatta National Hospital, Kenya: A cross-sectional study. BMJ open. 9(1):e023995. [Crossref] [Google Scholar] [Pub Med]
Kocalevent RD, Berg L, Beutel ME, Hinz A, Zenger M, Harter M, Nater U, Brahler E (2018). Social support in the general population: Standardization of the Oslo social support scale (OSSS-3). BMC Psychol. 6(1):1-8. [Crossref] [Google Scholar] [Pub Med]
Lee HS, Duffey KJ, Popkin BM (2013). Sodium and potassium intake patterns and trends in South Korea. J. Hum. Hypertens. 27(5):298-303. [Crossref] [Google Scholar] [Pub Med]
Lee PH, Macfarlane DJ, Lam TH, Stewart SM (2011). Validity of the international physical activity questionnaire short form (IPAQ-SF): A systematic review. Int. J. Behav. Nutr. Phys. Act. 8(1):1-11. [Crossref] [Google Scholar] [Pub Med]
Morrisroe J (2014). Literacy Changes Lives 2014: A New Perspective on Health, Employment and Crime. National Literacy Trust. [Google Scholar]
Nadewu AN, Geda B (2018). Adherence to healthy lifestyle among hypertensive patients in Harar region, eastern Ethiopia. Prim. Health. Care. 8(4):1-7. [Crossref] [Google Scholar]
Niriayo YL, Ibrahim S, Kassa TD, Asgedom SW, Atey TM, Gidey K, Demoz GT, Kahsay D (2019). Practice and predictors of self-care behaviors among ambulatory patients with hypertension in Ethiopia. PloS one. 14(6):e0218947. [Crossref] [Google Scholar] [Pub Med]
Obirikorang Y, Obirikorang C, Acheampong E, Anto EO, Amoah B, Fosu E, Amehere JA, Batu EN, Brenya PK, Amankwaa B, Adu EA (2018). Adherence to lifestyle modification among hypertensive clients: A descriptive cross-sectional study. Open Access Library Journal. 5(2):1-3. [Crossref] [Google Scholar]
Osako A, Chiang C, Ito K, Yatsuya H, Hilawe EH, Ikerdeu E, Honjo K, Mita T, Cui R, Hirakawa Y, Madraisau S (2017). Disparity in metabolic risk factors of non-communicable diseases between Palauans and Filipinos living in Palau. Nagoya. J. Med. Sci. 79(2):157. [Crossref] [Google Scholar] [Pub Med]
Oza R, Garcellano M (2015). Nonpharmacologic management of hypertension: what works? Am. Fam. Physician. 91(11):772-776. [Google Scholar] [Pub Med]
Perkovic V, Huxley R, Wu Y, Prabhakaran D, MacMahon S (2007). The burden of blood pressure-related disease: A neglected priority for global health. Hypertension. 50(6):991-997. [Crossref] [Google Scholar] [Pub Med]
Robbins CL, Dietz PM, Bombard J, Schmidt SM, Tregear M, Tregear SJ (2011). Peer Reviewed: Lifestyle Interventions for Hypertension and Dyslipidemia Among Women of Reproductive Age. Prev. Chronic. Dis. 8(6). [Google Scholar] [Pub Med]
Rossi A, Dikareva A, Bacon SL, Daskalopoulou SS (2012). The impact of physical activity on mortality in patients with high blood pressure: A systematic review. J. Hypertens. 30(7):1277-1288. [Crossref] [Google Scholar] [Pub Med]
Salam A, Atkins E, Sundstrom J, Hirakawa Y, Ettehad D, Emdin C, Neal B, Woodward M, Chalmers J, Berge E, Yusuf S (2019). Effects of blood pressure lowering on cardiovascular events, in the context of regression to the mean: A systematic review of randomized trials. J. Hypertens. 37(1):16-23. [Crossref] [Google Scholar] [Pub Med]
Sanabria-Ferrand PA, Gonzalez Q LA, Urrego M DZ (2007). Healthy life styles in Colombian health professionals: Exploratory study. Revista. Med. 15(2):207-217. [Google Scholar]
Svetkey LP, Erlinger TP, Vollmer WM, Feldstein A, Cooper LS, Appel LJ, Ard JD, Elmer PJ, Harsha D, Stevens VJ (2005). Effect of lifestyle modifications on blood pressure by race, sex, hypertension status and age. J. Hum. Hypertens. 19(1):21-31. [Crossref] [Google Scholar] [Pub Med]
Tagoe HA, Dake FA (2011). Healthy lifestyle behaviour among Ghanaian adults in the phase of a health policy change. Global. Health. 7(1):1-9. [Crossref] [Google Scholar] [Pub Med]
Tibebu A, Mengistu D, Negesa L (2017). Adherence to recommended lifestyle modifications and factors associated for hypertensive patients attending chronic follow-up units of selected public hospitals in Addis Ababa, Ethiopia. Patient Prefer Adherence. 11:323-330. [Crossref] [Google Scholar] [Pub Med]
Ukpabi OJ, Ewelike ID (2017). The eighth joint national committee on the prevention, detection, evaluation, and treatment of high blood pressure (joint national committee-8) report: Matters arising. Niger. j. cardiol. 14(1):15. [Crossref] [Google Scholar]
Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ (2018). 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 71(19):e127-e248. [Crossref] [Google Scholar] [Pub Med]
World Health Organization (2007). Reducing salt intake in populations: Report of a WHO forum and technical meeting, 5-7 October 2006, Paris, France. [Google Scholar]
Worku Kassahun C, Asasahegn A, Hagos D, Ashenafi E, Tamene F, Addis G, Endalkachew K (2020). Knowledge on hypertension and self-care practice among adult hypertensive patients at university of Gondar comprehensive specialized hospital, Ethiopia, 2019. Int. J. Hypertens. 2020:5649165. [Crossref] [Google Scholar] [Pub Med]
Xiao X, Wu ZC, Chou KC (2011). A multi-label classifier for predicting the subcellular localization of gram-negative bacterial proteins with both single and multiple sites. PloS. one. 6(6):e20592. [Crossref] [Google Scholar] [Pub Med]